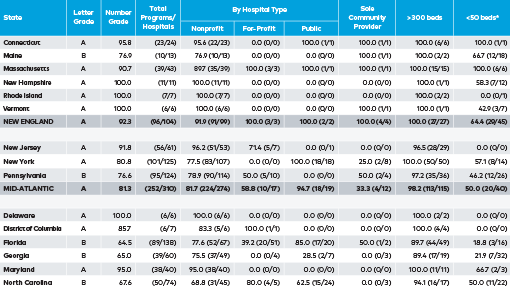
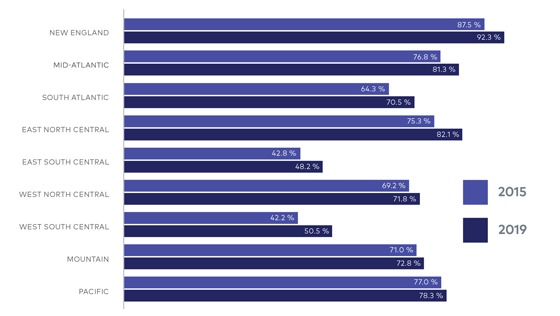
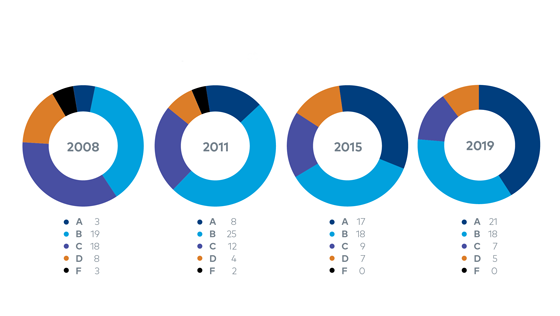
Since the last State-by-State Report Card was published (2015), the palliative care field has made steady progress across multiple domains, thanks in part to supportive policies from Congress, federal agencies, and state governments, as well as generous private sector investments. However, prevalence varies based on geography and hospital characteristics such as size and tax status. Leaders in the public and private sectors can take specific actions to standardize access to timely and high-quality palliative care services and move U.S. health care to a system that reliably meets the needs of people living with a serious illness, and their families.
Policy Progress over the Past Four Years
WORKFORCE GROWTH
Since the formal recognition of palliative care as a medical subspecialty in 2008, the field has grown to include 7,618 board-certified palliative care physicians,22 and more than 18,000 palliative care–certified nurses.23 The Social Work Hospice & Palliative Care Network (SWHPN) released a palliative care certification program in 2018, and specialty training and certification opportunities now exist for chaplains, physician assistants, and pharmacists.
PAYMENT REFORM
In the last three years, Medicare has made changes to allow specific payment for advance care planning and complex chronic care management. The Center for Medicare and Medicaid Innovation (CMMI) began testing new models that expand access to palliative care specialists, including the Oncology Care Model and the Medicare Care Choices Model. The Creating High-Quality Results and Outcomes Necessary to Improve Chronic (CHRONIC) Care Act, passed as part of the Bipartisan Budget Act of 2018, will allow Medicare Advantage (MA) plans to pay for social supports as well as in-home palliative care services for specific populations. Value-based insurance design may also provide a payment platform for non-hospital palliative care.
QUALITY, STANDARDS, AND RESEARCH ADVANCES
In 2015, the National Quality Forum (NQF) established a Palliative and End-of-Life Care Standing Committee (changed to the Geriatrics and Palliative Care Standing Committee in 2018) to rigorously scientifically review and endorse quality measures for older adults and those with a serious illness. In 2018, the Centers for Medicare and Medicaid Services (CMS) contracted with the American Academy of Hospice and Palliative Medicine (AAHPM) to develop new palliative care quality metrics to help fill measurement gaps identified by NQF. In 2018, the fourth edition of the National Consensus Project (NCP) Clinical Practice Guidelines for Quality Palliative Care was published, updating existing guidelines and establishing new standards and expectations for all health care professionals caring for people living with a serious illness, and their families. In the areas of research, the National Palliative Care Research Center and the National Institutes of Health (NIH) published white papers on palliative care research funding priorities, followed by a series of NIH program announcements encouraging submission of palliative care research projects. Concurrently, the Patient-Centered Outcomes Research Institute (PCORI) directed roughly $100 million to palliative care research, comparing the effectiveness of different delivery strategies across providers, settings, and modalities.
ENHANCED CLINICIAN SKILLS
Recognizing that nearly all clinicians care for patients living with a serious illness, several states passed laws for continuing education requirements in pain management, safe opioid prescribing, and palliative care. Several private health plans are beginning to require clinician training in core palliative care knowledge and skills as a component of their incentive programs for hospital quality.
INCREASED PUBLIC AWARENESS AT THE STATE LEVEL
As of publication, twenty-eight states have established Palliative Care Advisory Councils (or similar bodies) that are charged with increasing awareness of palliative care. Activities include developing websites to provide palliative care information to state residents, analyzing state-level access to palliative care, and providing state governments with recommendations for future policy action.
Remaining Gaps
Despite this progress, people living with a serious illness still do not have reliable access to palliative care. To ensure this access, policymakers must overcome persistent gaps and challenges.
WORKFORCE
Inadequate workforce and workforce pipeline to meet the needs of patients living with a serious illness, and their families
PAYMENT
Insufficient financing and financial incentives to ensure equitable and reliable access to palliative care for all people living with a serious illness
QUALITY, STANDARDS, AND RESEARCH
Lack of accountability for access to high-quality care delivery for patients with a serious illness; gaps in the evidence base to build the science guiding clinical practice
CLINICIAN SKILLS
Insufficient clinician training in communication; pain and symptom management; family assessment and support; and care over time and across settings
PUBLIC AND CLINICIAN AWARENESS
Continued lack of knowledge about the benefits of palliative care and who can benefit from it
Leaders in both the public sector (particularly those who oversee Medicare and Medicaid) and private sector (private health plans, purchasers, and accountable care organizations) can take specific actions to address these issues.