back to state reports index
Palliative Care in Maryland
OPPORTUNITIES TO IMPROVE PALLIATIVE CARE
ACCESS AND QUALITY IN YOUR STATE
| Location | 2019 Grade* | By Hospital Size | |||
|---|---|---|---|---|---|
| < 50 beds | 50-150 beds | 151-299 beds | 300+ beds | ||
| State | 95.0% A |
66.7% (2/3) |
92.9% (13/14) |
93.3% (14/15) |
100.0% (11/11) |
| Region | 70.5% B |
34.4% (44/128) |
52.8% (86/163) |
69.6% (103/148) |
93.2% (124/133) |
| National | 71.5% B |
36.3% (557/1535) |
51.1% (474/928) |
75.6% (578/765) |
93.7% (671/716) |
South Atlantic Region = DC, DE, FL, GA, MD, NC, SC, VA, WV
*The 2019 State-by-State Report Card on Access to Palliative Care in Our Nation’s Hospitals grade excludes hospitals that have fewer than 50 beds. Report Card grades are as follows: A (80% or more of hospitals with 50+ beds have palliative care), B (60-79%), C (40-59%), D (20-39%), F (less than 20%).
Hospital Palliative Care by Geography
Hospital palliative care is most common in urban communities. The graph below (figure 1) compares hospital palliative care availability in your urban, suburban, and rural communities against the regional and national percentages, and includes hospitals of all sizes.1
Hospital Palliative Care Availability in Maryland
The map below (figure 2) shows all Maryland hospitals that report palliative care, and includes hospitals of all sizes.1 Solid dots indicate hospitals that report palliative care programs and empty dots indicate hospitals that do not currently offer palliative care.
Figure 2. Availability of Hospital Palliative Care in Maryland
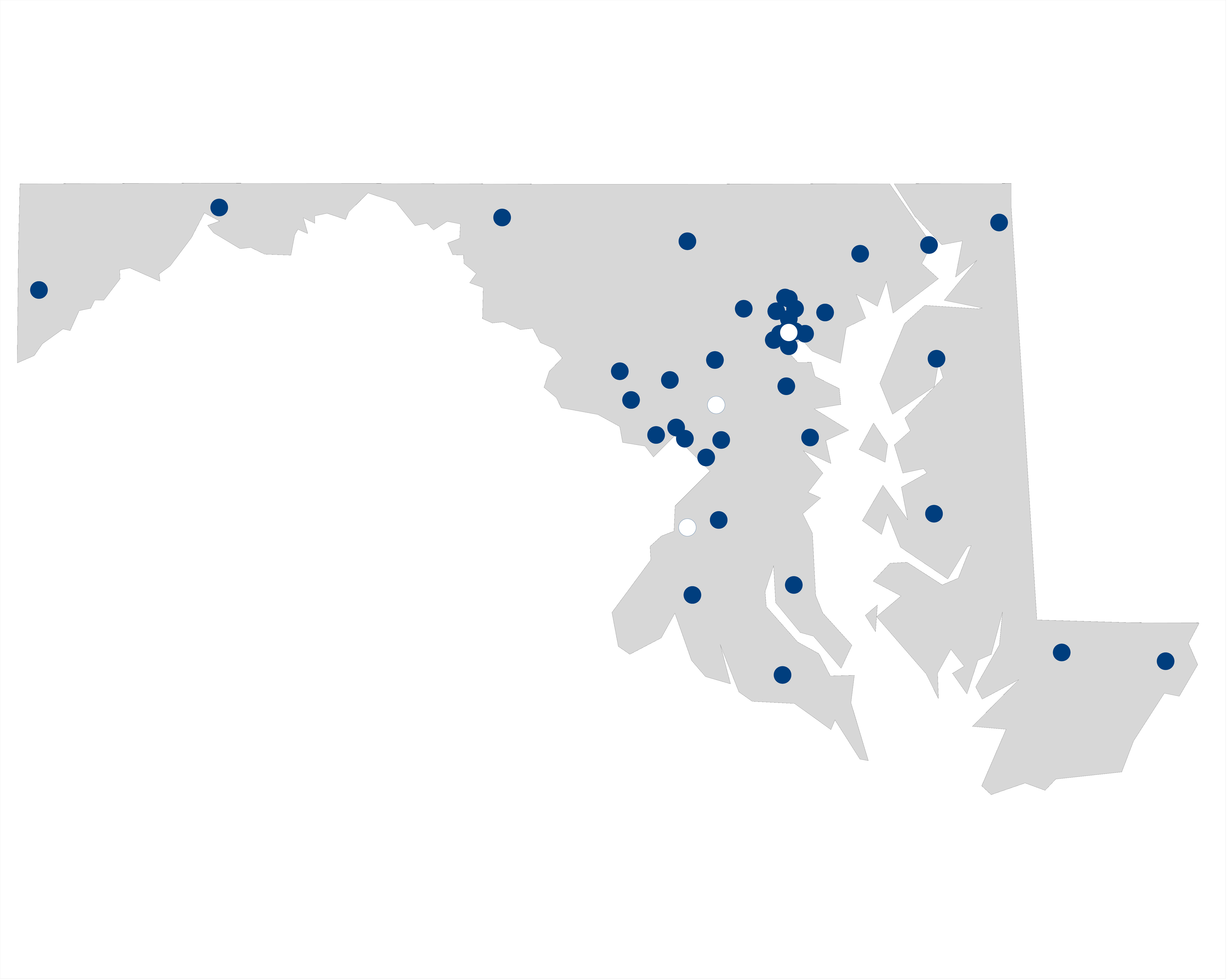
- No
- Yes
Community Palliative Care in Maryland
The Center to Advance Palliative Care (CAPC) also collects information on palliative care programs serving patients in office practices, clinics, nursing homes, and/or home-based settings.
At least 21 programs providing palliative care in the community have been reported in your state.3 Visit GetPalliativeCare.org for information on palliative care programs that have chosen to participate in the Provider Directory.
Certified Palliative Care Clinicians in Maryland
Physicians, advanced practice registered nurses, registered nurses, social workers, and chaplains can all pursue specialty certification in palliative care. Not all who work on palliative care teams have received palliative care certification, and there may be some palliative care–certified clinicians who work in other capacities.
The graph below (figure 3) shows the numbers of MDs, APRNs, and RNs who have received specialty certification in palliative care or pediatric palliative care.4 A number of palliative care–certified doctors of osteopathy (DOs), social workers, and chaplains may be providing care in your state, but these numbers were either unavailable or too low to be included at the state level. Additional members of the palliative care interdisciplinary team include physician assistants, pharmacists, and other health professionals as needed, although specialty palliative care certification does not currently exist in these fields.
There are 3.1 certified prescribing palliative care providers (MDs or APRNs) per 100,000 residents in your state.5 This capacity is likely insufficient to meet the needs of your state. Building the skills of all clinicians caring for people with serious illness may be an important strategy to complement the specialty palliative care workforce.
- Certified Physicians (MD): American Board of Medical Specialties (ABMS) Subspecialty Certification in Hospice and Palliative Medicine (including Pediatrics)
- Certified Advanced Practice Nurse (NP or CNS): Advanced Certified Hospice and Palliative Nurse
- Certified Nurse (RN or Pediatric RN): Certified Hospice and Palliative Nurse & Certified Hospice and Palliative Pediatric Nurse
Continuous Improvement Efforts in Maryland
In Maryland, 43 organizations are currently members of the Center to Advance Palliative Care, and have access to tools, clinical and operations training, and technical assistance in support of high-quality palliative care services.
This means that thousands of health care clinicians already have access to training in communication skills, pain and symptom management, supporting family caregivers, and building new palliative care programs. Contact membership@capc.org to discuss how you can leverage these resources.
CAPC State Recommendations
State champions can make a number of changes to advance palliative care access and quality in the areas of workforce, payment, clinician skill building, and public awareness. Examples of state initiatives include:
- Using state policies and regulations to define palliative care services and standards2
- Expanding or establishing new licensure to allow for the provision of home-based palliative care
- Establishing or expanding loan forgiveness programs for certified clinicians who work as palliative care specialists
- Enabling Medicaid to pay for high-value services beneficial to those with a serious illness by using existing codes, particularly advance care planning
- Adding palliative care coverage requirements in all settings to Medicaid managed care organization contracts, including special considerations for pediatrics, adolescent and young adult, and perinatal
- Enhancing Dual Special Needs Plans and Managed Long Term Services and Supports contracts to incorporate advance care planning and symptom assessment into care manager responsibilities
- Incorporating serious illness quality measurement reporting requirements and/or incentive programs into provider and managed care organization contracts
- Revising state health professional licensure and continuing education requirements to include a minimum number of hours of instruction in both communication skills and symptom management
- Investing targeted professional education opportunities in both communication skills and symptom management through grantmaking or other programs
- Increasing the role of state public health agencies in promoting palliative care by creating a public awareness campaign
- Conducting a state palliative care needs and capacity assessment (foundational to state work)
Palliative care leaders in this state may have more targeted recommendations to improve access and quality, and should be consulted before embarking on any new initiative. Visit CAPC’s State Policy Resources for more information and/or email paymentandpolicy@capc.org to join the State Palliative Care Forum.
Resources
- 2019 State-by-State Report Card on Access to Palliative Care in Our Nation’s Hospitals – scorecard.capc.org
- Mapping Community Palliative Care: A Snapshot – capc.org/mapping-community-palliative-care
- Communication and pain/symptom management training for all clinicians caring for patients with serious illness – capc.org/training
- CAPC federal and state policy resources – capc.org/policy-matters
- Serious Illness Strategies for Health Systems, Health Plans, and Accountable Care Organizations – capc.org/strategies
- Public information about palliative care – GetPalliativeCare.org
- Marketing and Messaging Palliative Care (including results from public and professional opinion surveys) – capc.org/marketingtoolkit
- National Academy for State Health Policy (NASHP) State Strategies to Address Palliative Care – nashp.org/nashp-resource-hub-state-strategies-to-address-palliative-care
- American Cancer Society Cancer Action Network – fightcancer.org/what-we-do/palliative-care
- Catalyst for Payment Reform Palliative Care Resources for Employers and other Health Care Purchasers – catalyze.org/product/palliative-care-purchaser-resources
- National Consensus Project Clinical Practice Guidelines for Quality Palliative Care, 4th edition – nationalcoalitionhpc.org/ncp
Citations
- Center to Advance Palliative Care analysis. See the 2019 State-by-State Report Card on Access to Palliative Care in Our Nation’s Hospitals for additional details on data sources and methods for hospital palliative care. https://scorecard.capc.org
- National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care, 4th edition. Richmond, VA: National Coalition for Hospice and Palliative Care; 2018. https://www.nationalcoalitionhpc.org/ncp
- Center to Advance Palliative Care analysis. See Mapping Community Palliative Care: A Snapshot for additional details on data sources and limitations for community palliative care. https://capc.org/mapping-community-palliative-care
- Information on certified palliative care clinicians come from:
- American Board of Medical Specialties (ABMS) Certifications (as of June 30, 2019) https://www.abms.org/media/257753/abms-board-certification-report-2018-2019.pdf
- Hospice and Palliative Credentialing Center (Nursing Certifications) https://advancingexpertcare.org/HPNA/HPCC/CertificationWeb/Certification_Verification.aspx?QueryMenuSelectedKeyctl01_TemplateBody_WebPartManager1_gwpciCopyofVerifyHPCCCertifications_ciCopyofVerifyHPCCCertifications=1a8a8414-8530-4518-8e61-b63932e17f9d
- Center to Advance Palliative Care analysis of physicians and nurses certified in palliative care per 100,000 residents per state. Population counts were obtained from the United States Census. https://www.census.gov/data/datasets/time-series/demo/popest/2010s-state-total.html
This report was prepared on 12/13/2019. Some of the figures may use data from earlier years.
Contact Us
Inquiries about the 2024 Serious Illness Scorecard should be directed to:
paymentandpolicy@capc.org
Media inquiries: Visit the Press page
Contact Us
Inquiries about the 2024 Serious Illness Scorecard should be directed to paymentandpolicy@capc.org
Suggested Citation: America’s Readiness to Meet the Needs of People with Serious Illness: 2024 Serious Illness Scorecard. Center to Advance Palliative Care. August 2024.